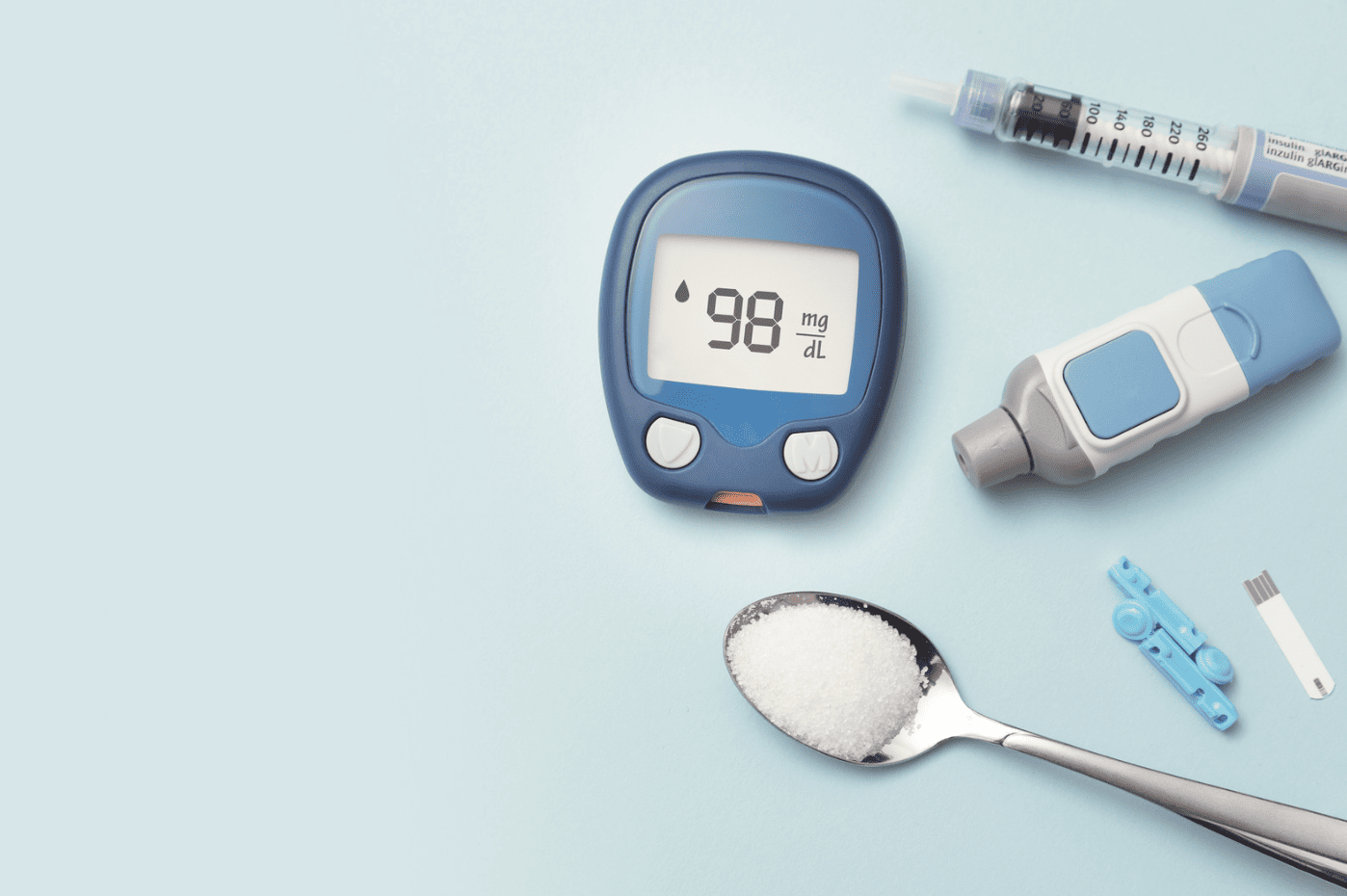
Diabetes is the seventh leading cause of death in the U.S. Beyond that, it can be mentally and physically exhausting to navigate. No matter the type, it demands that you take stock of your physical and mental health.
Working hand-in-hand with your healthcare provider is vital to your well-being. To make it a little easier, there are several apps to manage diabetes.
These apps can help you manage your diabetes with several key features. You can track your blood sugar levels and read content about diabetes. It can also support and motivate you, which is essential to the success of your diabetes management.
Today we’ll cover the types of diabetes, diabetes management apps, key features, and what app might be the best fit for you to manage your diabetes.
Types of Diabetes
Diabetes is a chronic disease that affects how your body turns food into energy. There are more than 133 million Americans living with diabetes or pre-diabetes. Each of the three types of diabetes varies in severity, symptoms, and the recommended course of management. Read on to learn about each type.
Type 1 Diabetes
Approximately 5% of people who have diabetes have type 1 diabetes. Otherwise known as juvenile diabetes, it is the most severe form of the disease. It typically develops in children and teenagers but can affect anyone, at any time, despite their age.
In type 1 diabetes, the disease causes the body to attack its cells. Specifically, the cells in the pancreas where insulin is made. Insulin is the hormone that helps the body use energy and manage glucose. Without proper insulin production, it can cause significant health problems – it has near-total beta cell destruction, leading to insulin dependence. Without proper insulin production glucose becomes stored in the blood stream, and rather than being distributed to the body’s cells, the body’s cells starve.
Symptom development can occur in as little as a few weeks or months and can escalate fast. Symptoms are typically too severe to ignore and must be managed immediately. If left untreated, type 1 diabetes can result in damage to the eyes, kidneys, nerves, and the heart, through uncontrolled high sugar levels. In the worst-case scenario, type 1 diabetes can lead to coma and death.
The causes of each type of diabetes are commonly confused. Type 1 diabetes isn’t caused by lifestyle or diet choices, but is instead understood to be caused by a combination of genetic and environmental factors.
Unfortunately, there is no cure for type 1 diabetes yet. But, it can be managed with insulin injections, blood sugar monitoring, and a well-rounded whole-food diet.
Type 2 Diabetes
The most common type of diabetes is type 2 – approximately 90% of people with diabetes have type 2. It is most commonly developed in adults after age 35 but is increasingly developing in younger adults.
Type 2 diabetes is typically related to adults that are overweight and have a sedentary lifestyle. It can take years for symptoms to develop and often go unnoticed. Thankfully, this type of diabetes can be managed by weight loss, diet, and increasing activity levels.
There are two types of dysfuncation that can happen which cause Type 2 diabetes. First, in insulin resistance the cells simply become resistant to the increased insuln being produced by the pancreas. Second, in beta cell dysfunction, the pancreatic cells aren’t able to keep up with the level of insulin production, and it causes blood sugar to rise. Both of these dysfunctions can be culprits and work together to cause Type 2 diabetes.
Type 2 diabetes can cause serious health problems including heart disease, vision loss, and kidney disease.
Gestational Diabetes
During pregnancy, your body goes through a lot of hormonal changes and creates more hormones. Every year, in approximately 2% to 10% of pregnancies in the US, pregnancies are affected by gestational diabetes.
Gestational diabetes functions similarly to type 2 diabetes in that it affects the way that your body’s cells use insulin. It creates insulin resistance in your body which increases your body’s need for insulin for it to function correctly. Approximately 50% of women with gestational diabetes will develop type 2 diabetes.
Gestational diabetes does not typically show symptoms – your doctor has to run a test for it. It is common for every pregnant woman to be tested at around 24 to 28 weeks gestation. This is when it is typically identified.
Gestational diabetes can be managed by diet and exercise, but may also require further intervention. Doctors may prescribe insulin, metformin, or another medication that can keep your blood sugar and insulin levels under control.
Diabetes Symptoms
You should speak with your doctor if you experience any of these symptoms:
- Frequent urination, especially at night
- Increased thirst
- Unexpected weight loss or difficulty gaining weight
- Increased hunger
- Blurry vision
- Numb or tingling hands or feet
- Very tired
- Very dry skin
- Slow healing sores
- Increased number of infections
Beyond these concerns, Type 2 and Gestational diabetes are harder to spot. They typically do not have any other symptoms. Type 1, however, can present with nausea, vomiting, and/or stomach pains.
Living With Diabetes
There are several things you can do to make life with diabetes a little easier, no matter the type. Here are some key things that you can do to help manage your diabetes:
- Be more active. Exercising regularly can positively impact your experience with diabetes. Exercise forces your muscles to use sugar (glucose) for energy and can help you manage your blood sugar.
- Food. Learn about carbohydrate counting and regulating food portion sizes. Carbohydrates have a large impact on your blood sugar levels. It’s important to know how many you’re consuming so you can manage your blood sugar level appropriately.
- Lower your stress. Hormones in your body go haywire when you’re stressed, and that can negatively impact your blood sugar level. Take note of your stress level on a scale of 1 to 10 every time to log your blood sugar level to identify any patterns.
- Take your medication (if prescribed). Consider the advice of your doctor or medical team, and be sure to take your prescribed medication as required. This can significantly impact your quality of life while living with diabetes.
The more you know about the factors that can influence your blood sugar level, the better you can prepare for fluctuations. If you are having difficulties getting your blood sugar level under control, reach out to your diabetes healthcare team for help.
Apps for People With Diabetes
Thanks to advances in technology, you’ve got one of the most powerful tools for managing your diabetes right in the palm of your hand. Your smartphone combined with a robust diabetes management app can make managing your diabetes much simpler. Read on to learn about apps to manage diabetes.
One Drop
One Drop is a diabetes management app that is available from the Apple Store and Google Play. Both the free and premium versions are available and have over 10 million downloads. This app offers blood sugar tracking, education on diabetes management, one-on-one coaching, and a community of others who are managing their diabetes. It can also help you set goals for your diabetes management.
Additional features in the premium version include health predictions that leverage AI to predict blood sugar levels in the future, trend analysis to give you insight into your blood sugar trends, and personalized coaching based on your individual needs.
Users can also purchase diabetes support items such as a glucose meter kit, a test strip plan, a body weight scale equipped with WiFi, and personalized coaching through the website to complement the app.
BlueStar Diabetes
The BlueStar Diabetes app is a unique digital coaching platform with guidance and insights based on clinical standards, that include FDA-cleared capabilities for type 1 and type 2 diabetes. A wide variety of features are available, including blood sugar tracking, educational resources such as articles, videos, quizzes, personalized coaching from certified diabetes care professionals, goal setting, and a collective community feature.
This app is available for free for Android and Apple devices. However, to activate the app, you need an access code from an authorized healthcare provider.
MyFitnessPal
Despite its reputation as just a calorie counter app, MyFitnessPal is so much more than that. It allows you to track your macronutrient intake, physical activity, and the timing of your meals. Users can set macronutrient goals that can significantly contribute to the ease of managing their blood sugar levels.
Although it doesn’t have a dedicated space for specifically tracking diabetes-related concerns, the app has a notes section where you can record blood sugar levels and insulin injections. MyFitnessPal also has a robust community feature to connect users. It can be a helpful tool for people looking to monitor their diabetes and improve their health.
The app has free and premium features and is available on the Apple Store and Google Play.
Glucose Buddy
Glucose Buddy helps people with diabetes manage their blood sugar levels. It allows users to track blood sugar readings, log meals, and gives nutritional insights. There is also a community forum where people can connect with others that are also managing diabetes.
The educational resources are robust. There is a 12-week diabetes education plan that users have access to. You can track exercise, food intake, and print out reports for your medical provider.
This app is available for Android and Apple users, however, there is no free version. Paid plans start at $19.99 per month. Higher-tier plans also include glucose testing strips and smart glucose meters.
Fresh Tri and Diabetes Patients
Fresh Tri was started with vulnerable populations in mind. Since its beginning, most of the team’s research has been centered around how to help disadvantaged populations and people dealing with chronic illnesses.
Part of managing diabetes requires a collaborative approach between the patient and the healthcare provider. A healthcare provider will suggest a recommended course of action, and a large part of the treatment plan for diabetes is diet and lifestyle change. Despite it being a critical piece of the puzzle, change can be hard.
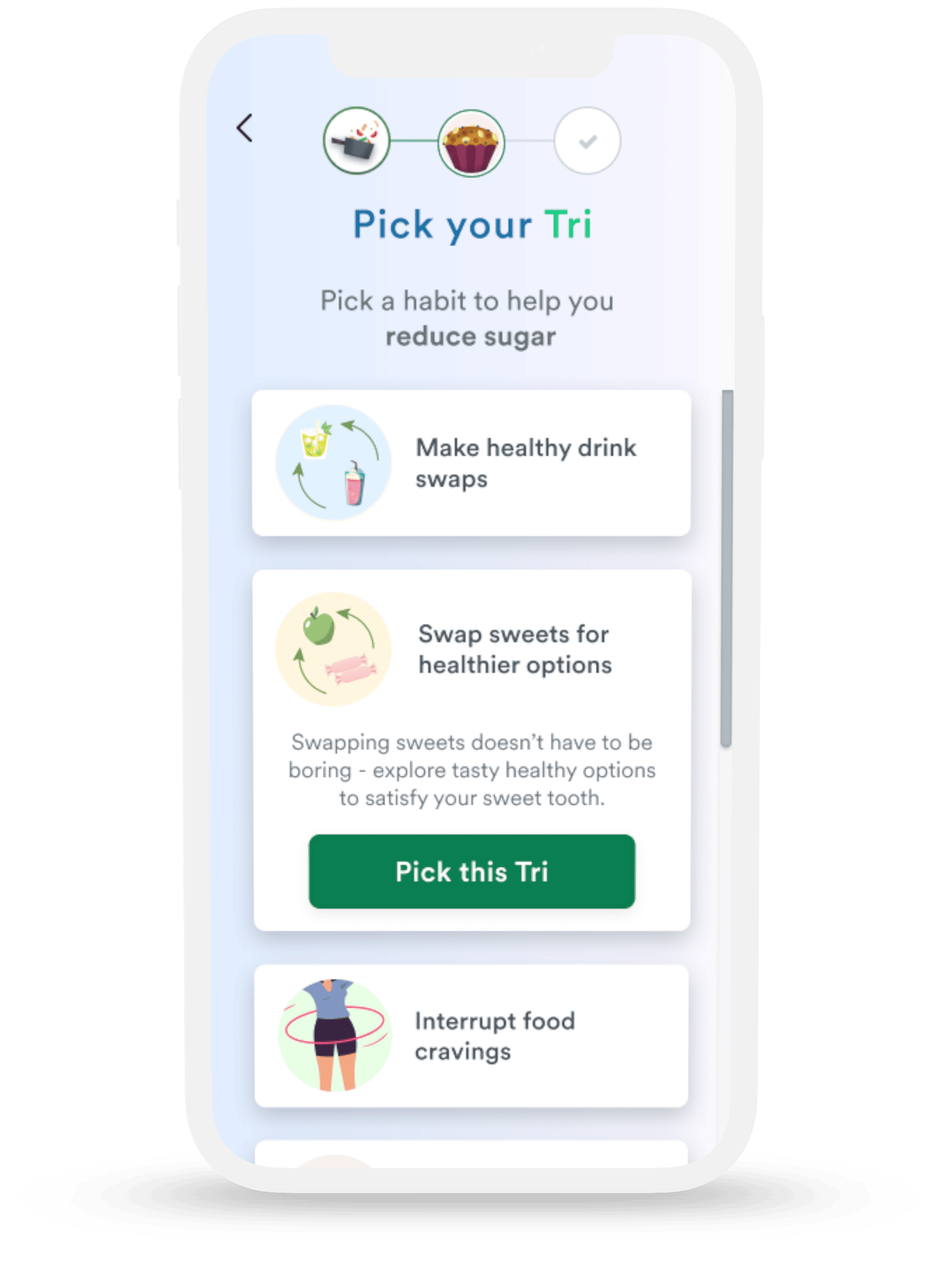
To support patients, Fresh Tri leverages research-backed neuroscience-based behavior modification techniques to assist people in reaching their wellness goals through the “Iterative Mindset Method” and the Fresh Tri app. By encouraging people to make small changes, called a “Tri”, Fresh Tri has been able to demonstrate statistically significant (p < 0.001) weight loss, habit formation, and improvements in mindset, persistence, and resilience in a recent study.
Using an app like Fresh Tri to help you iterate toward change and your health and wellness goals can make change feel a little less daunting. All of this can mean a greatly improved quality of life and increased ease of managing your chronic condition.
Try Fresh Tri to Manage Diabetes Symptoms
As we’ve discussed, diabetes can vary in type and severity and may require medication. Throughout your diagnosis, it’s vital to honor your primary healthcare provider’s recommendations above all.
Taking charge of your health and health goals is critical to the success of your collaborative care. You may feel overwhelmed and unsure of where to start, but there are helpful tools to help you succeed.
Fresh Tri is a helpful tool for people with diabetes. In partnership with their healthcare provider, Fresh Tri can help you track your progress on healthy habits, learn about diabetes and how to navigate the condition, connect with others in the community forum, and support you in your path to wellness.
Ready to Tri? Download the app to get started.